Goal setting is a game changer. Every healthcare organization has RCM milestones they want to hit or metrics they’d like to improve.
But how do you know if the goals of revenue cycle management you’ve set will make a real impact within healthcare today?
From protecting your foundation with key security checks to expanding denial prevention, here is your expert-vetted roadmap.
6 data-driven goals of revenue cycle management
- Security best practices
- Hospital price transparency
- Patient experience initiatives
- Denial prevention
- Medicare Advantage growth
- Technology checkup: AI/ML

GOAL 1: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Shore up security with 3 best practices
The case for shoring up security is simple: More than 132 million Americans were affected by health-record data breaches in 2023 alone. That’s roughly 40% of the U.S. population — and more than double the number of people who experienced breaches in 2022.
Meet this smart goal:
Secure three critical checkpoints:
- Review vendor access annually.
Companies are often attacked through vendors who have access to more data than they should. Limit vendors to minimum required access to reduce the likelihood of a breach. - Conduct a cross-functional ransomware tabletop exercise.
Many companies perform technical tests routinely and consider their system secure if they pass. But that excludes other teams — executives, legal, public relations — who must weigh in if a breach actually occurs. Conduct a cross-functional exercise to ensure you answer the necessary questions in advance. - Create a drawbridge protocol for B2B connections.
When a third party is infected, you need a fast way to break that connection — or “pull up your drawbridge” — until the threat is resolved. Just as with ransomware, build drawbridge plans now so you’re not making critical decisions in moments you could be taking action.

GOAL 2: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Comply with new hospital price transparency requirements
Since 2021, hospitals have been required to publicly post certain price and payer data in machine-readable files.
Now (as of January 1, 2024) CMS is taking that one step further by ensuring this data is displayed the same way across facilities so consumers can access and read it easily.
Meet this smart goal:
- Adopt the new CMS template
- Include an affirmation statement on your website
- Make this information easy to find
- Ensure your self-service tools are accurate
If you’re looking for an automated price transparency solution, pick one that’s market-tested to deliver answers in real-time. Simple, accurate tools will not only help you cultivate stronger patient loyalty but also increase cash flow.

GOAL 3: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Prioritize (the right) patient experience initiatives
Patient-facing financial processes have never been more critical.
So why are less than 7% of executives “very satisfied” with their technology in that department? Nearly half say insufficient automation is a top barrier to change in recent surveys.
With patient responsibility rising, it’s difficult to identify which actions will increase patient satisfaction and reimbursements.
Meet this smart goal:
- Educate your team.
Set standards for how to properly financially clear a patient. Provide detailed training and offer specific tips to help them collect with compassion at the point-of-service and after a visit. - Use technology to automate manual processes.
Implement solutions that are high-accuracy and low-touch first.- Run coverage discovery for eligibility transactions, or to solve denials when patients present as self-pay.
- Launch or optimize personalized, omni-channel communications.
- Send patient estimates prior to service via their preferred channel.
- Offer text-to-pay in addition to email and paper statements.
Implementing even one of these solutions will have an exponential impact on productivity and patient satisfaction.

GOAL 4: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Stop denials at these 4 key points
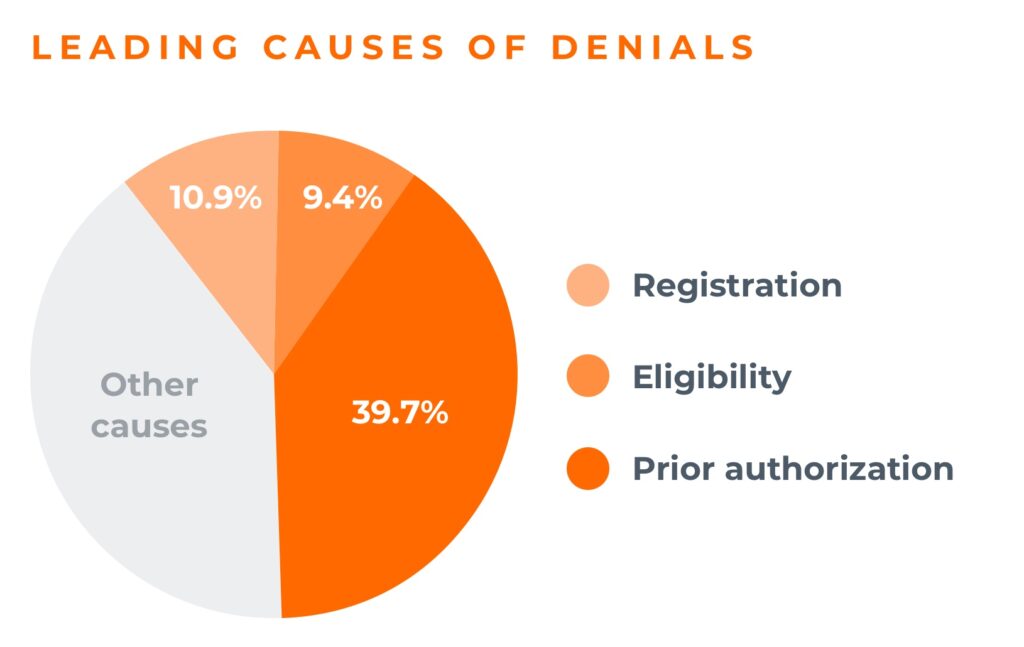
Research shows that 60% of denials come from the front end, and nearly 40% are caused by authorizations alone.
But if you put the right solutions in place at four key points, you can prevent denials before they happen.
Meet this smart goal:
- Use software to find more active insurance.
When 34% of patients who present as self-pay actually have active coverage, you can’t afford to let that revenue go. - Work by exception.
Use robust alerts and claim monitoring technology to work claims with a high probability of payment. That puts human efforts where they’ll matter most. - Arm managers with data and directives.
Build real-time dashboards to help managers identify root causes of denials. When managers can show other teams exactly what’s happening, it’s easier to shift from denial management to denial prevention. - Hold payers accountable.
Use payer scorecards to track where they’re impacting your cashflow. If a trend isn’t consistent with what you’re seeing from other payers, call that out.

GOAL 5: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Prepare for Medicare Advantage growth — and related denials
More than 33 million older Americans are enrolled in Medicare Advantage (MA) plans, wooed by lower premiums and more benefits than traditional Medicare. As that enrollment grows, providers should expect related denials to grow, too.
Why are those denials happening with Medicare Advantage?
- Insurers are denying claims due to lack of medical necessity.
While traditional Medicare is a straightforward payer category, MA plans have adopted more restrictive criteria commonly used among commercial payers. That’s led them to deny more inpatient hospital claims than all other payer types. - AI algorithms are wrongfully denying claims.
Some insurers are prioritizing faulty, profit-driven AI tools over doctor recommendations to decide how long patients need services, resulting in early coverage cutoffs. While 90% of these denials have been overturned, less than 0.2% of patients are actually choosing to appeal. And that leaves patients paying out of pocket or discontinuing post-acute care early. - Operational requirements are different from traditional Medicare.
Reports found that MA plans have, at times, delayed or denied beneficiaries’ access to medical care — even though the requests met Medicare coverage rules. They also denied payments for services that met both Medicare coverage rules and their own billing rules, such as MRIs and stays in post-acute facilities.
Meet this smart goal:
Make sure your team understands the potential denials impact for MA plans and implement solutions to mitigate those effects.
Automate:
- Prior authorization
Find a solution that automatically verifies, initiates, statuses, and retrieves comprehensive auth details — and ideally automates patient referral status to cut manual work. - Medical necessity checks
Look for a solution that auto-generates Advance Beneficiary Notices or Notice of Non-Coverage forms.

GOAL 6: REVENUE CYCLE MANAGEMENT IN HEALTHCARE
Quality-check your tech
Artificial intelligence (AI) and machine learning (ML) are key to optimizing end-to-end transactions, from processing more volume to improving patient outcomes. But as you implement them, ensure your partner or internal teams are delivering what they promised.
Meet this smart goal:
Perform a quality check. Ask:
- Is this technology scalable and secure?
It’s great to have a model that derives insight, but if it can’t handle your data load and output your information appropriately, you’re not going to get full value. - How large are the data sets we can access for this project?
Data-model performance is directly related to the size of the data set used to train that model. Make sure your data covers as many bases as possible. - What’s the use case for this model?
Models can’t be trained on data alone. Identify decision makers and people who can act as subject matter experts to help structure your model properly, reduce risk, and increase the likelihood of success. - How are we implementing automation within workflows?
The best models accurately predict outcomes, and real value comes from combining that information with strategies to change that outcome. That must happen inside workflows.
Ready to see a specific Waystar solution in action?
Discover the way forward.



