Numerous studies have shown that social determinants of health (SDoH) undoubtedly impact consumers’ health status, outcomes, and total cost of care. As care teams, provider organizations, and payers attempt to mitigate the impact of these non-clinical risk factors, understanding the consumer’s perspective on SDoH issues will be critical.
We surveyed 500 consumers to understand their individual SDoH contexts and any impact on medical encounters at a hospital or physician office — and compiled that feedback to identify opportunities for hospitals and health systems looking to improve patient engagement and social determinant challenges. The survey focused on recognized core SDoH categories: financial insecurity, social isolation, housing insecurity, addiction, transportation access, food insecurity, and health literacy.
Two major takeaways from our survey results were:
As suspected, there is a relationship between SDOH and health management, and
Healthcare organizations are falling short on properly implementing SDoH factors into practice
Overview
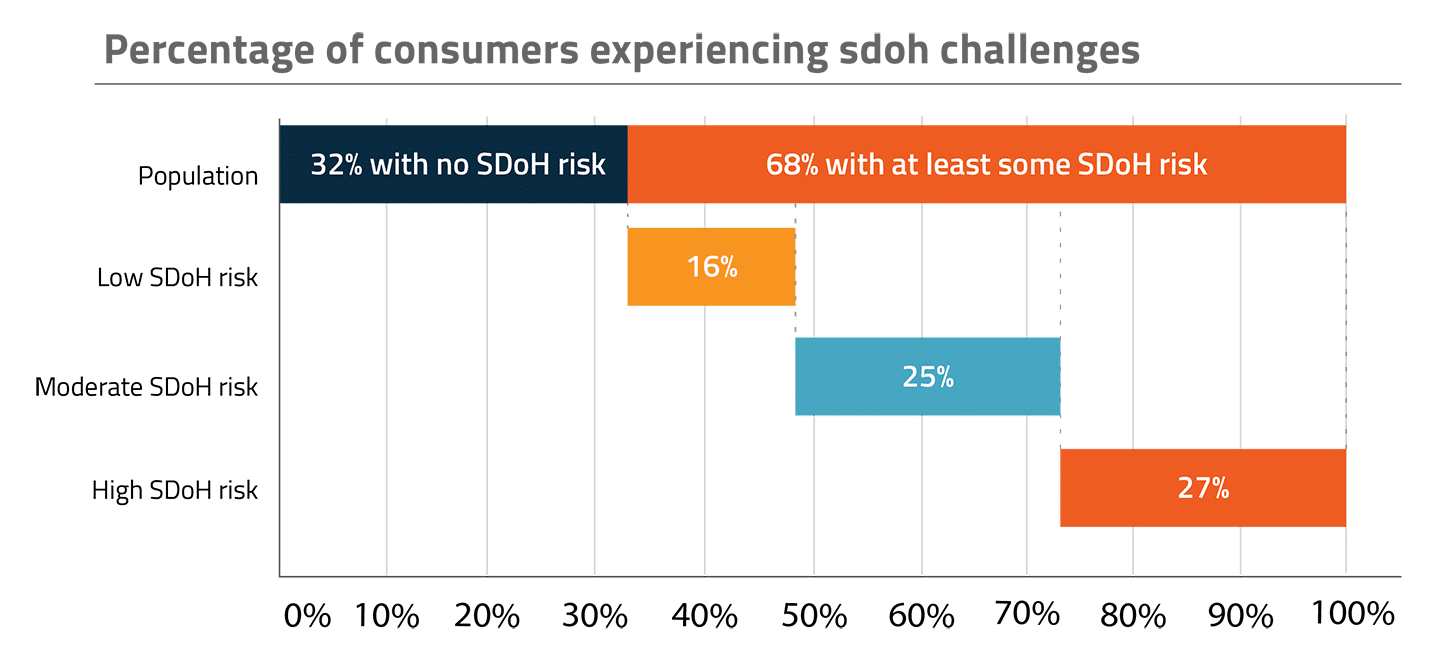
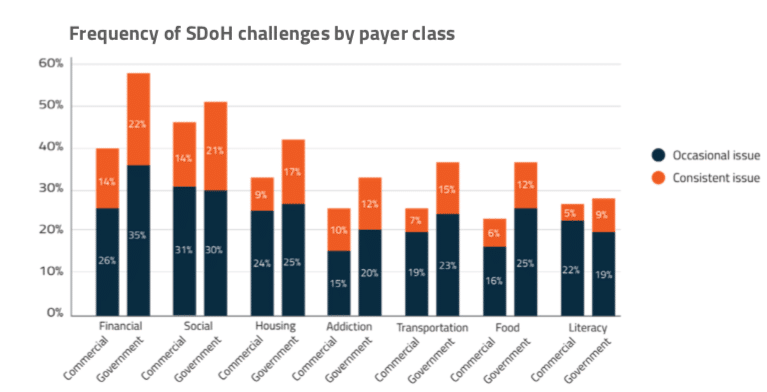
To get a better understanding of the population affected by social determinant challenges, we took a closer look at SDoH prevalence and composition (Figure 1.1). We found that SDoH risk is present across payer classes and social determinant challenges are common, with 68% of consumers having at least some level of SDoH challenges and 52% having moderate to high SDoH risk in at least one of the categories mentioned above. The most commonly reported SDoH issues are financial insecurity and social isolation (Figure 1.2).
Health status and SDoH challenges correlate
Individuals with SDoH stress rate their overall health status much lower than the overall population and are significantly more likely to suffer from one or more chronic conditions. Specifically, those with high SDoH stress are nearly 50% more likely to suffer from chronic conditions and 2.3X more likely to rate their health as “fair” or “poor.” Interestingly, even in the healthiest categories, more than one in five self-report high SDoH risk.
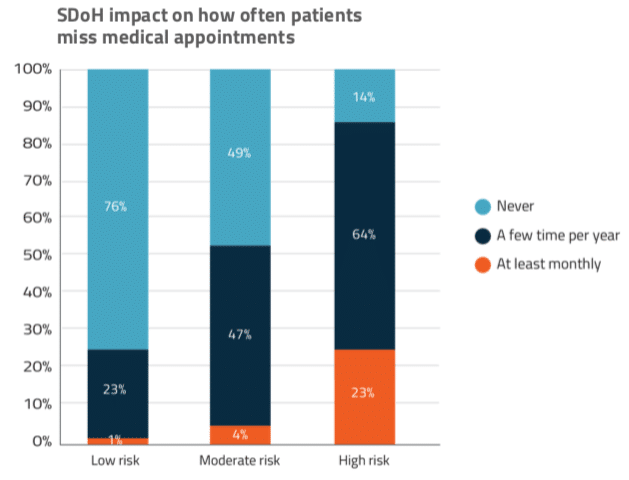
SDoH prevalence impacts the ability to get and stay healthy in tangible ways: patients with high SDoH risk are over three times more likely to miss multiple medical appointments per year (Figure 2.1).
Efforts to identify the prevalence of SDoH and engage patients
Providers and payers are beginning to utilize screening tools to understand SDoH challenges — typically a survey of approximately a dozen questions that are either completed by the patients themselves or administered by a member of the care team. This effort is far from universal due to issues of response and perception bias as well as resource limitations.
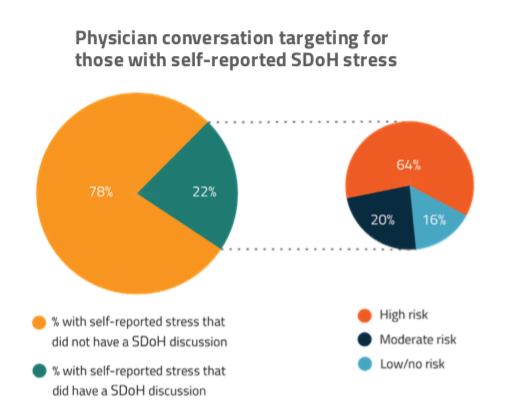
Only 22% of consumers with SDoH stress indicated having discussed these issues with their physician (Figure 3.1). Although roughly one in five patients with SDoH stress will have the conversation, the data suggests many risky patients are slipping through. Of all patients in the “high risk” segment, 60% never discussed their issues with a provider or their insurance company.
Patients with SDoH issues are 2.5X more willing to talk about those issues with clinicians compared to payers. Interestingly, 10% of respondents with commercial insurance and 20% of the respondents on Medicare or Medicaid prefer not to discuss SDoH challenges at all, highlighting the need for tactful, unobtrusive strategies for gathering social determinant insight.
As SDoH risks are identified, many organizations haven’t yet developed the necessary programs, services, or community partnerships required to address the needs of their patients. Even for those with the resources, it can be challenging to get patients to engage (Figure 3.2).
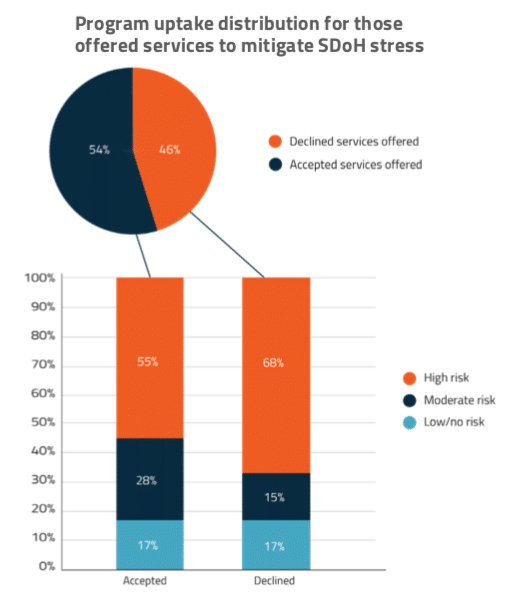
Most conversations about SDoH are occurring with patients that are least likely to have health issues and least likely to utilize support services, if available. Younger consumers (27 to 39-year-olds) are nearly twice as likely to have been engaged in a discussion of their SDoH challenges by their provider or insurance company. Unfortunately, they are also less receptive to assistance than the older segment (40 to 65-year-olds)
The opportunity
Figuring out how to engage patients in their SDoH challenges is core to successful, cost-effective, and high-value population health management. However, current efforts are still limited and have inefficacies such as unevenly applied targeting or done in a way that consumers choose to reject today. It’s clear that organizations have begun to collect SDoH data on some of their patients, but it is far from universal. It is therefore difficult to put into a consistent workflow when the information will only be available for a small portion of the patients they are treating.
As a first step, organizations need to talk with their care teams on the front lines to understand the gap they have in understanding the SDoH needs of their patients. Then they must figure out how best to gather that information at scale across their full population. A promising solution to this is technology utilizing predictive data analysis, which can segment patient populations without manual survey efforts, enable pre-arrival preparations, and suggest more appealing methods for program uptake. Waystar is already working on such technology that can also incorporate SDoH insight into available systems to ensure it’s accessible to all care team members across the continuum of care. This allows organizations to modify workflow to leverage these analytics in support of more accurate targets of highest-risk patients, more effective methods of engagement, and more efficient allocation of human and financial resources.


