This is the sixth post in a new Waystar blog series: 7 steps to sharpen your healthcare revenue cycle.
Can’t wait for a new blog each week? Download the eBook to learn 7 steps for maximizing your healthcare RCM software.
Denials in healthcare are an ever-present — and ever-increasing — problem. In 2022, denials in healthcare rose to 11% of all claims — up nearly 8% from the year prior.
It’s a particularly troubling issue when you know just how many denials in healthcare are preventable.
But how, exactly, do you ensure your organization is proactively preventing and managing denials? Start with four steps.
Preventing Denials in healthcare STEP:
1. Know the most common denial points
Denials in healthcare happen for any number of reasons, but many stem from errors or omissions at one of the following points:
- Registration
Incorrect coverage detection or data - Medical necessity
Procedure code isn’t supported by the diagnosis(es) - Timely filing
Claim wasn’t submitted to the payer within the required time frame - Pre-authorization
Payer didn’t grant authorization to perform the service - Duplication
Claim has been submitted more than once - Additional information
Payer requires extra information from provider or patient to process the claim - Coding
Service was not coded in accordance with the payer’s rules, or a combination of codes was used that the payer deems unpayable
Because payer rules are constantly changing, denials in healthcare will always be a moving target — particularly because payers have an economic incentive to deny claims. But that’s also one reason many organizations find automated denial and appeal management so effective.
Preventing Denials in healthcare STEP:
2. Implement practices to reduce denials
Despite the obstacles, efforts to prevent denials in healthcare are certainly worthwhile.
Start with the basics
- Know the payer’s payment policies to deter denials related to medical necessity.
- Integrate rules within your EHR system, as appropriate, to help prevent problems.
- Inform a patient about a denial, and address it in real-time, to improve the patient financial experience and care delivery.
Get creative with specifics
For example, if you know a certain insulin pump is likely to be denied by a patient’s insurance, make room to shift your plan. Knowing this, a proactive provider will prescribe a pump made by another manufacturer to avoid that denial altogether.
Preventing Denials in healthcare STEP:
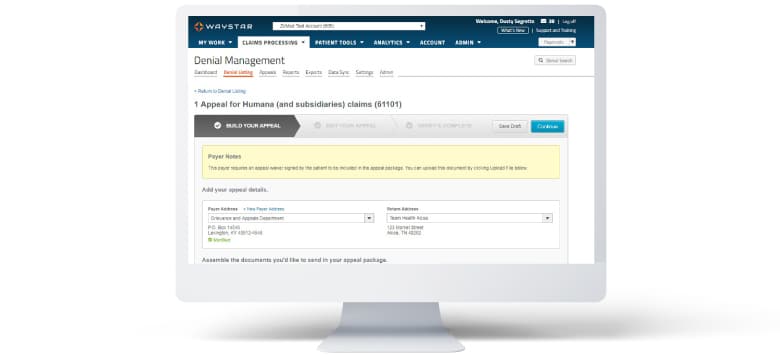
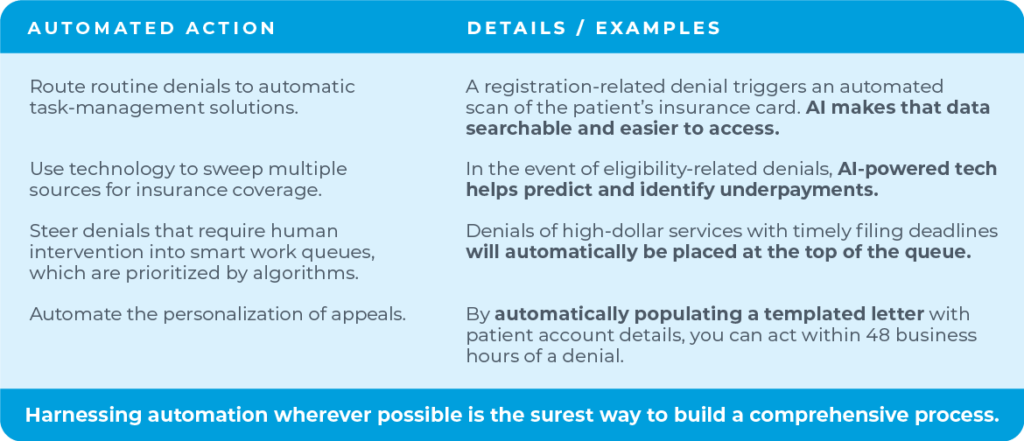
3. Build a complete, automated denials process
A timely, comprehensive process is key to managing denials once they happen, and that must include automation.
Automated action: Route routine denials to automatic task-management solutions.
Example: A registration-related denial triggers an automated scan of the patient’s insurance card. AI makes that data searchable and easier to access.
Automated action: Use technology to sweep multiple sources for insurance coverage.
Example: In the event of eligibility-related denials, AI-powered tech helps predict and identify underpayments.
Automated action: Steer denials that require human intervention into smart work queues, which are prioritized by algorithms.
Example: Denials of high-dollar services with timely filing deadlines will automatically be placed at the top of the queue.
Automated action: Automate the personalization of appeals.
Example: By automatically populating a templated letter with patient account details, you can act within 48 business hours of a denial.
Harnessing automation wherever possible is the surest way to build a comprehensive process for managing denials in healthcare.
Preventing Denials in healthcare STEP:
4. Track + report denials
Whether your organization is more focused on denial prevention or management, tracking is crucial.
To do it well, you must systematically capture the reasons for denials.
- Most are remitted electronically, but don’t ignore the denials that come in via direct correspondence with payers.
- Create a process that captures and reports the root causes of denials. Cataloging will enable you to monitor denials by type, frequency, value, and payer.
- Establish a team or workgroup to address denials and report on trends.
If you stick with this process, it will reveal critical opportunities to make your revenue cycle run more smoothly.
Want to know more about sharpening your rev cycle?
- Read all the blogs in this series
- Watch the webinar with Dr. Elizabeth Woodcock
- Download the complete eBook