Telemedicine and Medicare reimbursements are top-of-mind for healthcare organizations in 2025. With so many moving pieces, the changes can be difficult to navigate.
However, Dr. Elizabeth Woodcock shines a light on the complexities to help guide providers forward.
“For more than 30 years, I’ve been tracking what happens in the reimbursement and payment landscape,” says Dr. Woodcock, DrPH, MBA, FACMPE, CPC. “There’s a lot of change coming in 2025, and there’s no better time to talk about it than now.”

Telemedicine reimbursement in 2025: How organizations can prepare
Since the 1980s, patients have had to live in healthcare deserts for their providers to get reimbursed for virtual care. During COVID-19, the government expanded that access — but that expansion ends March 31, 2025.
“We’re at an inflection point for telemedicine,” says Dr. Woodcock. “There’s a law on the books for virtual care, and because the Centers for Medicare & Medicaid Services (CMS) can’t change the law, they’re still relying on regulatory power to keep telemedicine reimbursable.”
Think of it like a speed limit: If a road is under construction, the city can temporarily change the speed limit to keep people safe. But once that construction is over, the city can’t make that temporary change permanent; the government has to do it. That’s where we are with telemedicine.
Know what’s permanent: Telemedicine in 2025
Going forward, reimbursement will apply to telemedicine provided:
- By federally qualified health centers (FQHCs) and rural health clinics (RHCs)
- Using audio-only services if the patient can’t or won’t consent to video
- By clinicians using enrolled practice locations to provide care, even if the care is performed elsewhere (for example, from their home)
“If you’re a provider of telehealth in 2025, be sure to leverage virtual check-ins for patient interactions that don’t require an in-person visit,” says Dr. Woodcock. “These visits are reimbursable, and they help maintain patient engagement, improve efficiency, and capture revenue.”

Stay ahead of changes: Telemedicine in 2025
- Adopt the latest CPT codes + know payer protocol in your market
Despite virtual care’s uncertain future, the American Medical Association (AMA) has replaced phone-based codes for many services (audio-only visits, new versus existing patients). If you don’t use the proper CPT code, your reimbursement is at risk. - Know your state laws
Determine what services may revert to pre-COVID rules in your state. - Analyze the value of telemedicine for your organization
Consider reimbursement but also patient and provider satisfaction.
Medicare reimbursement rates in 2025: What providers need to know
Medicare reimbursement rates in 2025 are a major concern for healthcare providers.
FACT #1: The Medicare conversion factor (CF) is down 2.83%
With the decrease from $33.29 to $32.35, providers are going to feel pressure, especially in settings where demand is high and care is scarce.
“This is bad news for us in healthcare,” says Dr. Woodcock. “There is an incredible supply-and-demand imbalance for provider services. There are so many waitlists, and nobody can get an appointment. That makes access to care really tenuous.”
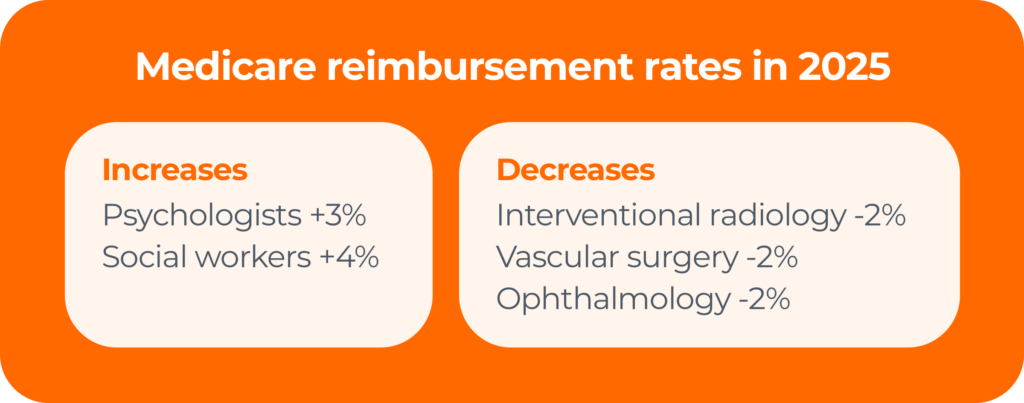
There are a few winners for Medicare reimbursement rates in 2025 — psychologists and social workers — but there are also a handful of providers that use the same set of CPT codes that will experience a 2% decline. That includes radiologists, vascular surgeons, and eye doctors.
FACT #2: Physician reimbursements have been in decline for decades
An AMA study found that reimbursement for physician services has dropped by nearly one-third (33%) over the past 25 years. This decline has occurred despite the fact that the costs of running a practice — salaries, tech updates, compliance — have skyrocketed.
Medicare updates compared to inflation in practice costs (2001–2025)
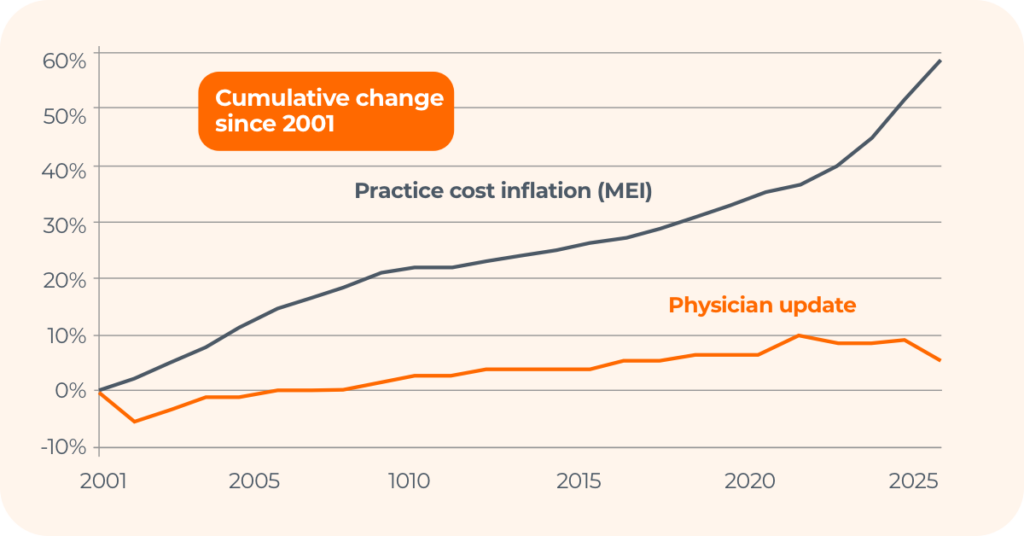
While there was a bill to counteract these cuts — the Medicare Patient Access and Practice Stabilization Act — it ultimately didn’t pass.
FACT #3: Sequestration will remain in place through 2030
Here’s a brief timeline of Medicare sequestration (the automatic, across-the-board spending cuts to federal programs):
- April 2013: Sequestration takes effect, reducing Medicare payments by 2%.
- May 2020 – March 2022: Congress suspends sequestration during COVID-19.
- April 2022 – 2025: Sequestration suspension is phased out.
Today, the full 2% sequestration is back in effect for all Medicare payments.
What can providers do?
- Use the Physician Fee Schedule search tool to see how these changes affect you.
- Consider diversifying your payer mix to reduce reliance on Medicare reimbursements.
Medicare services in 2025: What providers need to know
Medicare changes have ripple effects across the healthcare industry.

In 2025, Medicare reimbursements rates will increase for:
- Brain and mental health services, including FDA-cleared digital treatment devices
- Atherosclerotic cardiovascular disease (ASCVD) risk assessment and management
- Certain colorectal cancer screenings (CTC, blood-based biomarker)
- Hepatitis B vaccinations without an order
- Infectious disease care on the professional services side
5 steps to take to secure Medicare payments
- Consult the Medicare preventive services quick reference chart
Find out what’s covered, get related codes, track time limitations, and more. - Use CPT codes as much as possible
If you’re not using the proper CPT codes for services rendered, the codes may disappear. “CPT codes are use it or lose It,” says Dr. Woodcock. “Otherwise, what we’re signaling is that nobody is doing the work, and CMS will take them away.” - Claim payments for Advanced Primary Care Management (APCM)
If you provide primary care management for patients with one or more chronic conditions and meet certain requirements, use the following CPT codes to receive up to $110 per month per patient.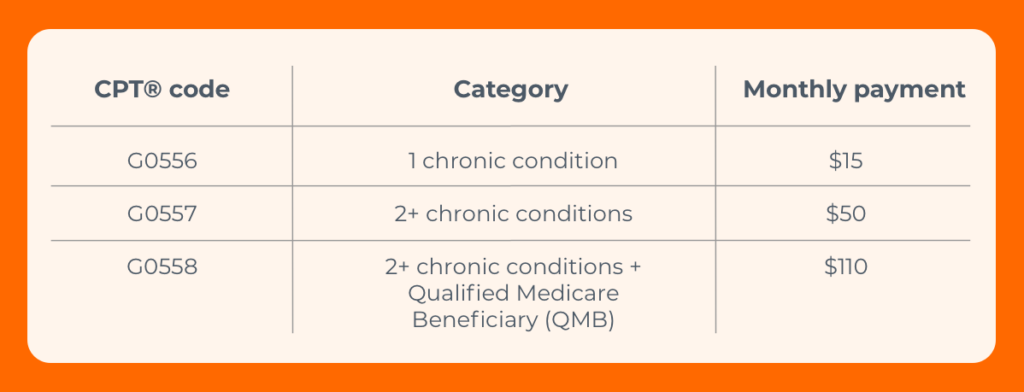
- Know where you stand with the Quality Payment Program (QPP)
- 2024 was the last year for any payment boost
- There have been changes to 66 current measures plus 7 new ones
- If you see CARC 237 or RARC N807, you could be penalized up to 9%
- Track changing and new CPT codes (including 270 new codes this year)
3 key takeaways for telemedicine, Medicare reimbursement rates + more in 2025
1. The healthcare industry is in the midst of massive changes
- Mergers and acquisitions are on the rise
Large health organizations will continue to grow, which affects the whole industry. - The physician shortage will get worse before it gets better
By 2036, the U.S. is projected to experience a shortage of 86,000 physicians according to the Association of American Medical Colleges. - The new presidential administration will heap change upon change
With new heads of both the Department of Health and Human Services (HHS) and CMS, change is the foregone conclusion.
2. The gateway to healthcare is now digital
“The front door to healthcare is changing,” says Dr. Woodcock. “It used to be us picking up a phone to call a provider. Today, it’s using digital tools that offer virtual health first. We’ve got ChatGPT, AI, Best Buy and Amazon Health, urgent care, and EHR systems that allow us to chat with our doctor without a copay.”

That’s leading to huge changes. Claim volumes are:
- Growing for retail clinics (200%) and urgent care (70%), but
- Shrinking for hospital ERs (1%) and primary care physicians (13%).
“What this means is we have to make sure we’re in the digital game,” says Dr. Woodcock. “We can’t go back and shut the door that COVID-19 opened. We’ve got to respond to our consumer.”
Make digital-first transactions work for you
Start with Patient Payments. Waystar clients have achieved a 30% increase in patient collections and 61% self-service pay rate on average using our integrated software.
3. Insurance payers still have the advantage
The pandemic tipped the scales in favor of payers.
“Claim volumes were lower during that time, but insurers didn’t reduce premiums,” says Dr. Woodcock. “So, patients continued paying while payers paid out less to providers.”
That’s still affecting providers today. Not only were margins low for years on end, but denials became an even bigger issue, with hospitals and health systems spending nearly $20 billion annually trying to overturn denied claims.
Stop the bleeding with automation, AI + GenAI to combat denials
When reducing denials is the #1 priority for providers, the right software is vital. See what Denial + Appeal Management can do for you, and how Waystar is leveraging generative AI to autonomously draft appeal letters with AltitudeCreate™.


