Today’s healthcare revenue cycle landscape is undergoing significant transformations. From shifting payer policies and skyrocketing denials to heightened concerns around data security, the challenges providers face grow more and more complex.
With $440 billion spent on healthcare administrative work every year, decision-makers are embracing new advancements in the healthcare revenue cycle — including artificial intelligence (AI), software innovations, and strategic partnerships — to drive efficiency and protect their organization’s financial health, now and in the future.
In collaboration with Qualtrics, Waystar conducted a recent market survey of more than 600 healthcare revenue cycle leaders, garnering exclusive insights that reveal the top investment priorities and strategic focus areas for 2025. Here are the top takeaways from the report — and ways your own health organization could see meaningful results.
TOP PRIORITY FOR RCM LEADERS
1. Investing in AI + GenAI capabilities to fuel efficiency + cost savings
In the healthcare revenue cycle, AI and generative AI (GenAI) are no longer just buzzwords — they are critical tools to maximize efficiency amid obstacles like rising transaction volumes and increasing costs.
Survey data reveals that 92% of respondents indicate their top priority is to invest in or further implement AI, generative AI, and automation for revenue cycle management. Additionally, findings from a 2024 report show 100% of healthcare leaders see the benefit of AI in revenue cycle management.
Waystar recently launched AltitudeAI™, a comprehensive set of capabilities designed to elevate productivity and precision for healthcare providers at scale. This includes Waystar’s own generative AI-powered innovation — AltitudeCreate™ — which launched within Waystar’s Denial + Appeal Management solution.
This innovation has specifically enabled Waystar clients in the autonomous creation of appeal letters. Clients have already seen powerful results, including producing appeal packages three times faster, averaging 70% in time-savings.
WATCH NOW: The foundation and future of AI + generative AI in the revenue cycle industry
TOP PRIORITY FOR RCM LEADERS
2. Prioritizing RCM software that drives measurable ROI + financial performance
With so many industry pressures, it’s imperative to ensure that investments in healthcare payments software translate into tangible returns. According to survey results, 96% of providers consider strong ROI a top factor when purchasing new RCM software.
Furthermore, if current RCM software does not demonstrate desired outcomes or financial gains, healthcare leaders are quick to consider a new platform. In fact, software with low ROI ranks fourth in the top five reasons to switch to a new RCM partner.
“We know positive ROI is generated when we implement artificial intelligence,” said Chris Schremser, Chief Technology Officer of Waystar, during a 2024 keynote presentation The Foundation and future of AI + generative AI in healthcare payments.
With shifts in the healthcare revenue cycle landscape, AI and advanced automation remain powerful success factors to optimize financial performance and deliver long-term value.
CALCULATE NOW: See how much you could be saving with a platform approach to healthcare payments
TOP PRIORITY FOR RCM LEADERS
3. Safeguarding data against cybersecurity breaches
The February 2024 healthcare cybersecurity breach marked a turning point for revenue cycle leaders. After the most significant and consequential data breach in U.S. healthcare history, the protected health information (PHI) of 184 million individuals was compromised.
In the wake of this incident, safeguarding data and cybersecurity have become even more paramount for healthcare organizations. In fact, healthcare finance leaders cite data security concerns as a top reason they would consider switching RCM software vendors.
“You’ve got to have the critical infrastructure in place to be able to leverage data in a smart, responsible way. The underpinning of this is security; software providers must deliberately choose to secure their platform and be steadfast in achieving compliance,” shares Schremser.
WATCH NOW: Waystar security spotlight: A platform designed for trust
TOP PRIORITY FOR RCM LEADERS
4. Adopting end-to-end platforms over point solutions
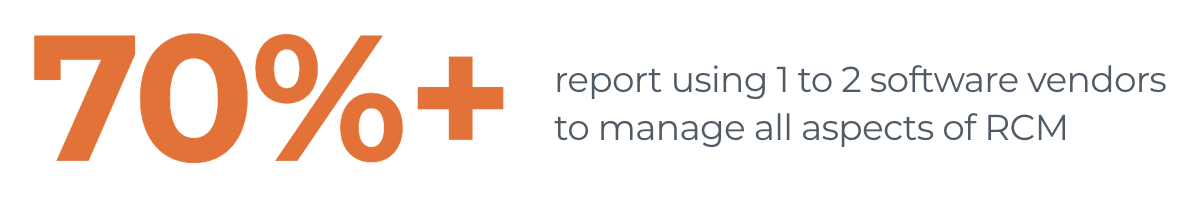
Healthcare organizations are turning away from standalone solutions in favor of adopting end-to-end software platforms to address revenue cycle challenges. While relying on individual point solutions may have provided temporary relief in the past, they often lead to long-term inefficiencies and operational bottlenecks.
Research shows a 70% YOY increase in the adoption of end-to-end platform strategies. By shifting from fragmented solutions to end-to-end software platforms, providers can optimize performance across the revenue cycle, leveraging advancements in AI and automation.
With a platform strategy approach, data flows seamlessly from patient access to the final reimbursement, ensuring that all financial and clinical information remains accurate and consistent throughout the complete revenue cycle.
READ REPORT: Accelerate performance with an RCM platform strategy
TOP PRIORITY FOR RCM LEADERS
5. Enhancing patient access to boost precision + prevent denials
Every year, hospitals and health systems spend nearly $20 billion attempting to overturn denied claims. Furthermore, 60% of providers report their top pain point for denials stems from the frontend patient access processes, including prior authorization, registration, and eligibility.
Today’s providers understand that one of the most effect forms of denial prevention is ensuring upfront accuracy of all information at the beginning. Waystar’s Authorization Manager is helping healthcare organizations like Prisma Health improve authorization accuracy and speed.
“Prior authorizations are one of our biggest administrative challenges. By collaborating with industry partners on innovative processes that deliver high-impact solutions, we are able to make a significant difference for our organization and help provide better care for our patients,” shared Patrick Griffin, Executive Director of Revenue Cycle at Prisma Health.
EXPLORE MORE: How Waystar Authorization Manager increases speed and accuracy
TOP PRIORITY FOR RCM LEADERS
6. Strengthening cash flow with error-free claim submissions
When it comes to RCM functional areas, streamlining claim management to prevent denials continues to be a major focus. That’s because automating claim management workflows directly impacts a healthcare organization’s reimbursement speed, accuracy, and overall financial performance — along with their ability to fuel their mission.
With payers continually adjusting policies and procedures, automating claims is no longer optional. Leveraging AI and advanced automation in the claim management process ensures claims are submitted accurately the first time, leading to quicker reimbursements and stronger financial performance.
Explore the top trends in the healthcare revenue cycle for 2025
Read our latest report for RCM strategies to stay on the forefront of shifts in the healthcare payments industry.