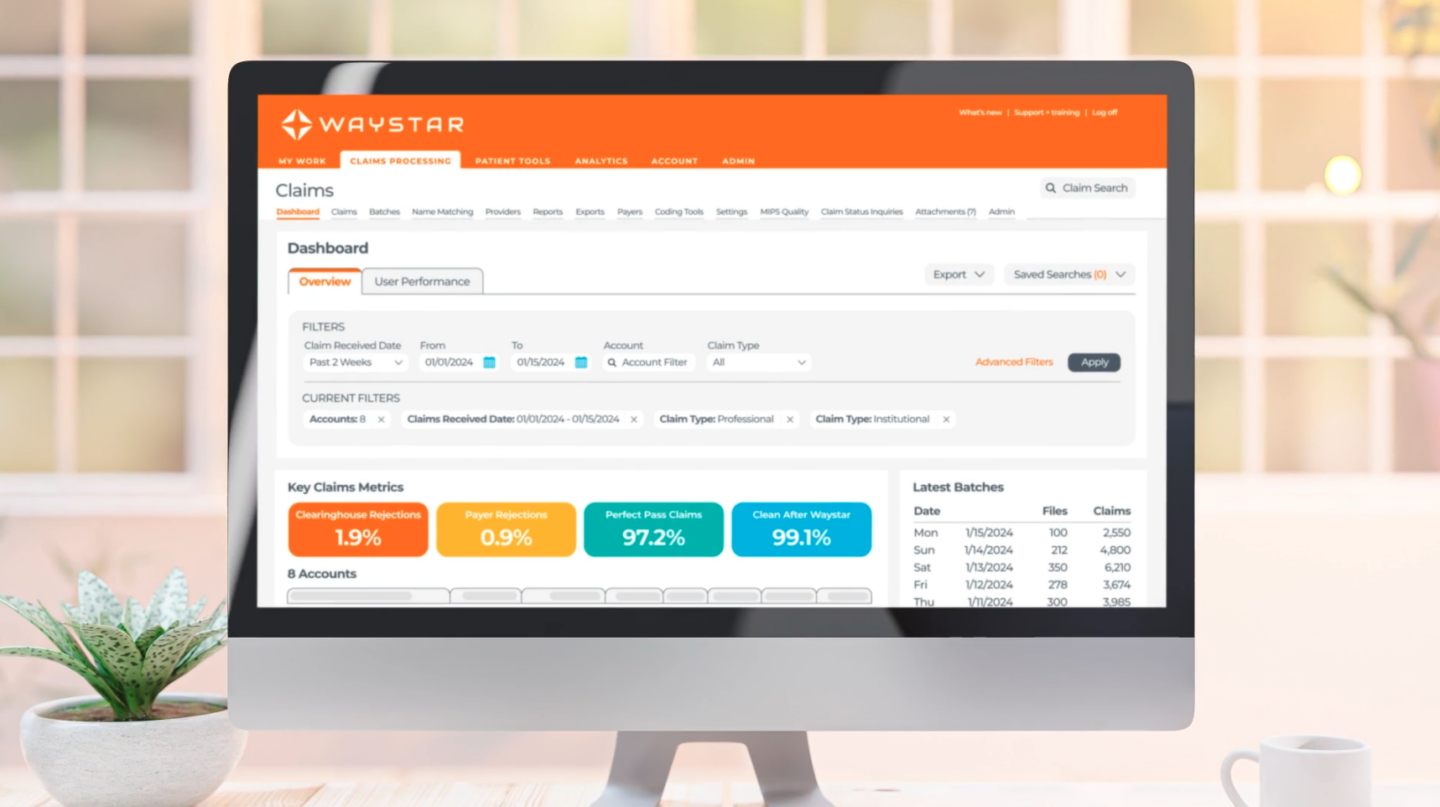
Prior authorization delays are the #1 cause of claim denials. Waystar’s Authorization Manager streamlines workflows, reduces manual work, and speeds up approvals for organizations like Frederick Health — so patients get care faster.
“What gets me excited is the Waystar authorization tools,” says Shawn McCardell, AVP of Revenue Cycle at Frederick Health. “They automatically check and submit the authorizations so my team can focus on the core things they need to do: denials and appeals. It ultimately provides a better patient experience throughout the whole revenue cycle”
It’s time to minimize rework and maximize results.