Today’s healthcare leaders encounter a variety of challenges when it comes to payments — from patient expectations and government policies to labor shortages and increasing claim volumes. Meeting these challenges head-on requires forward thinking, namely the use of artificial intelligence (AI) in RCM.
A recent study, Examining AI adoption + ROI in healthcare payments, evaluated the role of artificial intelligence in improving RCM processes. Modern Healthcare and Waystar joined forces to survey 68 healthcare leaders and professionals about:
- The role of AI
- Where it’s making an impact today, and
- How healthcare organizations hope to use it in the future.
Here are just three highlights from the study that leaders need to know now.
1. FACT: AI in RCM yields positive ROI
AI implementation can improve claim accuracy from the start, helping teams bring in faster, fuller payments.

It’s easy to see the positives associated with applying AI to the revenue cycle. Every health executive surveyed agreed that AI can bring value to healthcare revenue cycle management. But while leaders understand the benefits of using AI, there are barriers to entry. The top is cost, according to 75% of those surveyed, followed by security concerns (65%), and the ability to integrate within their existing EHRs and PMs (65%).
And then there’s the overarching question every leader must answer: Will the organization see returns?
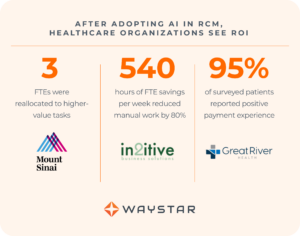
According to the study, early adopters say “yes.” Most survey respondents (75%) who use AI already see a return on their investment.
More about security + AI in RCM
2. FACT: AI in RCM increases efficiency
Using AI to cut manual RCM tasks gives healthcare professionals more time to focus on patients.
It’s no secret that many RCM tasks are repetitive, transactional, and time-consuming. AI can help alleviate all those problems.
Automating tasks related to claim management, eligibility verification, and even authorizations allows teams to work by exception only. In other words, the software takes on the bulk of the repetitive tasks so your team only needs to spend time on tasks outside the norm. With this change, teams can shift their focus to:
- Only work on high-level initiatives, and
- Spend more time focusing on the patient.
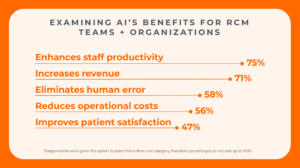
With efficiencies implemented throughout the revenue cycle, real change can be tracked and measured. Study respondents agree, with 75% saying that AI enhances staff productivity.
Looking at specific examples of this in action, automated technology can help shave:
- 17 minutes off each claim status inquiry, and
- 16 minutes off each eligibility check.
With the high volume of claims coming through each day, time saved quickly adds up.
More about generative AI in RCM
3. FACT: AI in RCM has extensive capabilities in healthcare
Generative AI can improve efficiency and accuracy in specific areas across the revenue cycle — and healthcare leaders are ready to use the new technology.
AI is poised to change the landscape of healthcare payments, inspiring leaders to explore ways the software can make a positive difference. They’re also taking that to the next level with generative AI, technology that learns and creates new content based on prompts and inputs from users
Waystar is working with Google Cloud to use generative AI to address some of the U.S. healthcare system’s most complex and critical challenges.

In one use case, Waystar and Google Cloud automated the extraction of prior authorization requirements from complex payer data sets. In a proof-of-concept study by Waystar, the application:
- Reduced the time to generate an authoritative report of procedural preauthorization by 99.93% while
- Increasing accuracy by 13%.
This is just one example of the powerful results AI can deliver.
Dive deep into GenAI in RCM
Learn more about the possibilities of AI in healthcare RCM
Download the full report from Waystar and Modern Healthcare, plus explore real-world examples of successful implementation.



