Denial + APPEAL Management
Resolve denials. Recover more revenue.
When decreasing denials is the #1 priority for providers, healthcare denial management software is vital.
Denial + Appeal Management harnesses the power of AI and advanced automation to resolve denials faster and recover more revenue with less manual effort. By leveraging generative AI to autonomously create appeal letters and simplifying the process with pre-populated, payer-specific forms, our software platform helps you overturn more denials — and even prevent them in the first place — while maximizing reimbursement and efficiency.

Proven healthcare denial management software
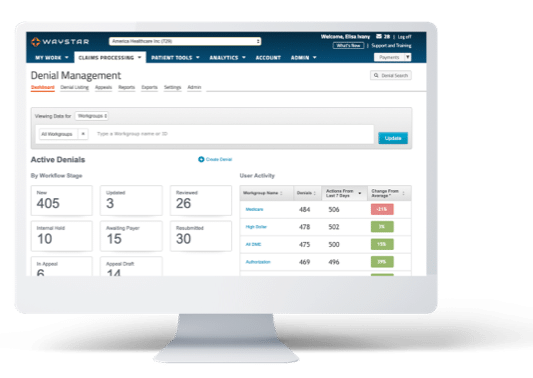
Speed + maximize reimbursement
Denial + Appeal Management uses Waystar’s extensive data sets to prioritize denials likely to result in payment and automatically route them to the right work groups using AI and advanced automation. It leverages a library of 1K+ prepopulated payer-specific forms and the power of generative AI to effortlessly generate and submit appeal packages. Our software does all this while integrating directly into your EHR, HIS or PM.
Denial + Appeal Management offers:
- AI + predictive analytics to prioritize the denials most likely to be overturned and paid leveraging Waystar AltitudeAI™
- Autonomously generate appeal letters using generative AI with Waystar AltitudeAI™
- A 100% paperless process + batch appeal submission options to increase efficiency
- Appeal tracking + proof of delivery to eliminate uncertainty
- Customized, exception-based workflows to meet your unique needs
- Advanced analytics + root-cause reporting to support decision-making and denial prevention
- Automatically verify and identify updated coverage information for eligibility-related denials using Auto Coverage Detection, accelerating collections and reducing denial follow-up
ACCELERATE APPEALS + MITIGATE DENIALS
Leverage AI to expedite appeals
Using powerful generative AI capabilities, Waystar AltitudeAI™ effortlessly creates appeal letters with unprecedented speed and accuracy, helping you recover a substantial portion of payments with less manual lift.
to create 100
appeal packages
overturn rate with
AltitudeAI™
Transform your revenue cycle with Waystar
Use our smart software platform to get even more out of healthcare denial management software — all through a single, cloud-based experience.
Complementary Solutions
Claim Manager | Claim Monitoring | Claim Attachments | Coverage Detection | Analytics + Reporting

Connect with a denial management software expert
Discover how Denial + Appeal Management can optimize your workflows to stay ahead of denials and get paid faster. Fill out the form below, and we’ll be in touch shortly.