
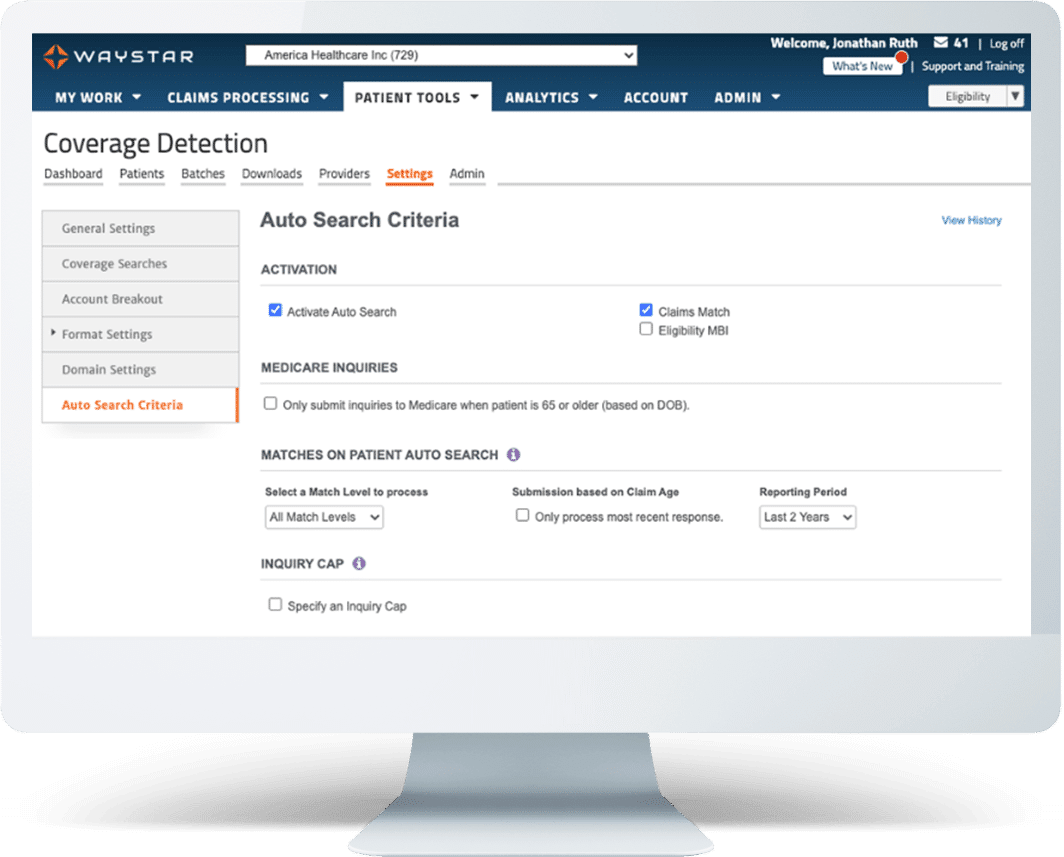
COVERAGE DETECTION
Find coverage other solutions won’t
Discovering hidden coverage is vital to protecting your financial standing. But with providers feeling the margin squeeze, they must ensure identifying active, billable coverage is quick, seamless, and drives considerable ROI.
With Waystar, detection has never been simpler.
Our Coverage Detection solution makes confirming active coverage fast and efficient. Capturing billable insurance that might otherwise be overlooked will help your organization generate more income while relieving the financial burden that would have been placed on patients.
WHAT MAKES WAYSTAR DIFFERENT
Make coverage detection fast + effective
Waystar’s software solutions leverage our expansive claims and eligibility databases, as well as a wealth of payer data to find more coverage — more accurately — and with less effort. Our cutting-edge technology:
- Automatically confirms active coverage regardless of patient’s point of entry
- Offers customizable dashboards and reports for billable transparency
- Provides actionable results for active and inactive coverage
- Maximizes efficiency with real-time responses
- Initiates Coverage Detection from Eligibility solution automatically
How much coverage are you missing? Take our quiz to learn how you’re doing with coverage detection best practices and what steps you can take to help your organization.
Smart coverage detection by the numbers

Solve your financial clearance puzzle with AI + automation
When it comes to financial clearance, healthcare organizations face many challenges from different directions. Rather than focus on one piece of the puzzle, create a holistic patient financial clearance strategy. Then execute it with the help of front-end revenue cycle automation for results that make a difference.

Coverage detection resources
Dig deeper into coverage identification
Solve your financial clearance puzzle with AI + automation
Diving into denial prevention with AI, appeals + more
Learn more about Waystar’s Coverage Detection solution
Learn more about Waystar’s Auto Eligibility + Coverage Detection solution
Get even more out of Waystar
The comprehensive Waystar platform offers a single sign-on for a full suite of solutions that work together to transform your revenue cycle. Click below to learn more about the solutions that complement Coverage Detection to help you increase revenue while offering the best possible patient experience.
COMPLEMENTARY SOLUTIONS
Eligibility Verification | Patient Estimation | Charity Screening | Claim Management | Advanced Propensity to Pay
Talk with a Coverage Detection expert
Let’s explore how we can automate your coverage detection processes and find coverage patients might not even know about. Fill out the form below and an expert will be in touch shortly. We look forward to talking with you!