
Eligibility Verification
The smart + simple way to verify eligibility
If you’re like most providers, your patient access team probably spends a serious amount of time verifying eligibility and benefit details for accuracy. Despite all this, 60% of providers cite frontend processes like eligibility as a top cause of denials that drain the bottom line.
Waystar’s Eligibility Verification automates much of this process so you can say goodbye to the days of searching and interpreting patient coverage and focus on what really matters — your patients. With our powerful technology at your fingertips, you can:
- Prevent more rejections and denials
- Strengthen frontend collections
- Optimize staff productivity
- Elevate the patient payment experience
ELIGIBILITY BY THE NUMBERS
TRUSTED BY HEALTHCARE LEADERS NATIONWIDE
WHAT MAKES WAYSTAR DIFFERENT
Powerfully accurate eligibility verification
Eligibility Verification combs through vast amounts of payer data to curate the most accurate and comprehensive benefit information — with richer coverage detail, staff become specialized in triaging eligibility issues. What’s more, our eligibility engine seamlessly integrates with all major EHRs.
Features + benefits
- Better defined, more detailed eligibility results with expansive payer connectivity
- Plan code matching to mitigate registration errors
- Normalization of payer data for more actionable, efficient workflows
- Intelligent alerts with actionable guidance for staff
- Automated initiation of Coverage Detection to find additional coverage in real-time
- Automatic searches to the correct payer if additional coverage is indicated
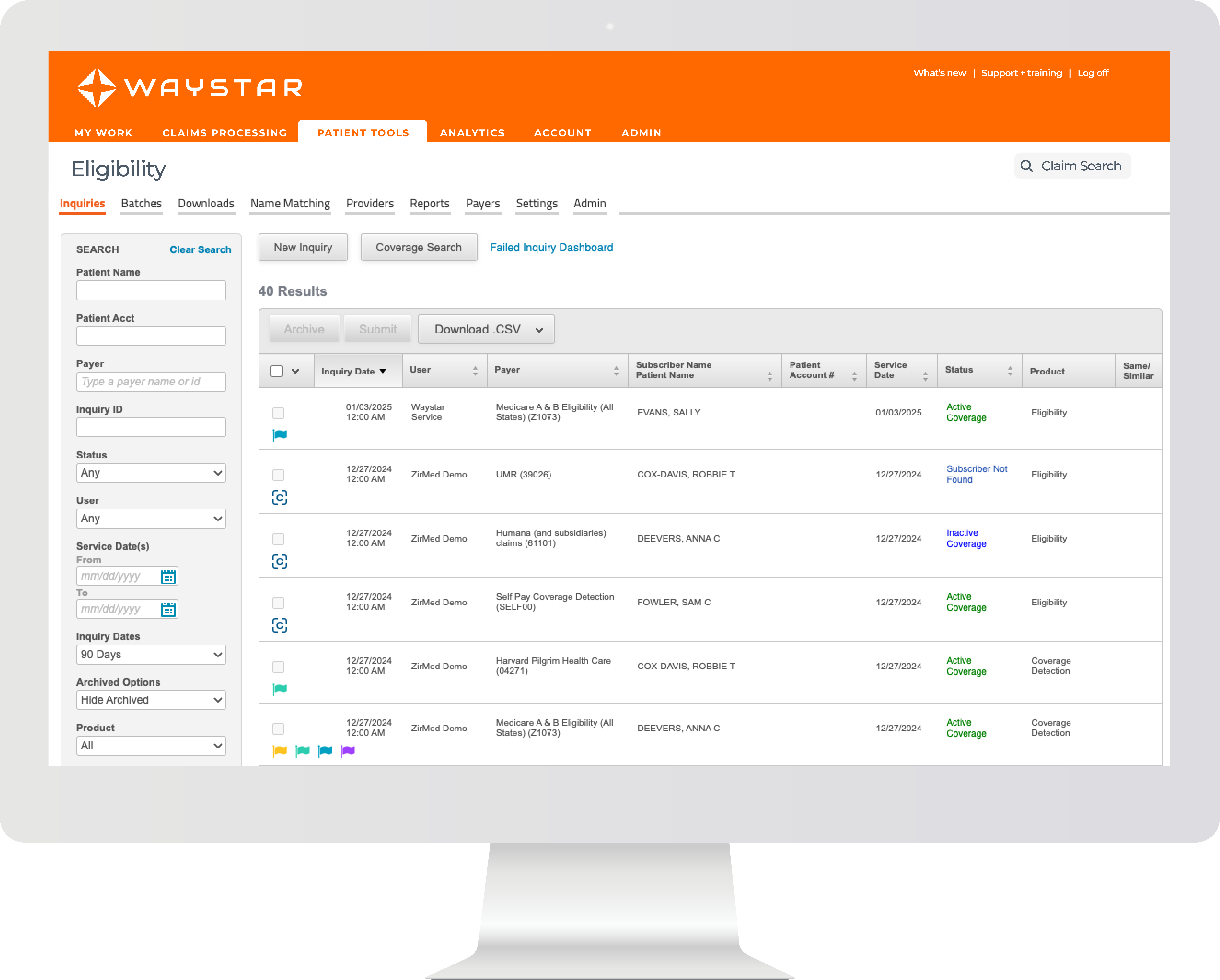
Complete + enriched benefit info in seconds
Getting insurance verification right the first time is crucial. Incorrect or incomplete eligibility has a ripple effect across the revenue cycle, from missed authorizations to reworking denied claims. Here’s a closer look at how our automated solution works.
Enriched benefit data
- Leverage our expansive data network, which houses more than 50% of the U.S. patient population, to find coverage and verify eligibility
- Utilize RPA and EDI connections to surface complete response
- Expansive payer connectivity is leveraged for best data in the market
- Detailed responses provide nuanced benefits information for improved accuracy
Automated, intelligent workflow
- Auto Coverage Detection searches for hidden or unknown coverage in real-time, without manual intervention
- Integrated workflow for seamless user experience
- Intelligent, actionable warnings and alerts for patient MBIs and managed Medicaid plans
- Guided next best user actions help you navigate for optimized results
Unparalleled financial clearance operations
- Auto-rechecks eligibility whenever account data is updated
- Benefit information is normalized for ease of consumption
- Payer connectivity monitoring provides visibility into payer health and automatically finds alternate routes in the event of payer outages that make direct connectivity unavailable
Get valuable insights into eligibility verification
Mastering eligibility: 3 essential strategies for a resilient revenue cycle
Waystar’s Eligibility Verification provides actionable, accurate data in real time
How verifying insurance eligibility can increase revenue + ease staff burden
How Prisma Health empowers their team and boosts productivity

Solutions that augment Eligibility Verification
Our solutions work together seamlessly to help bring even more value to your organization. Realize even greater benefits by exploring solutions especially complementary to Eligibility Verification below.
COMPLEMENTARY SOLUTIONS
Authorization Suite | Coverage Detection | Patient Estimation
Talk with a solution expert about Eligibility Verification
We want to hear from you about your organization’s challenges and needs. Fill out the form below to learn more or ask questions about Eligibility Verification — and how we can work together to help your team reduce denials and maximize collections.



